
The Caregiver-Provider Gap: Why Communication Breaks Down and How to Bridge It in 2026
1.1.26
Caregivers and providers are often working toward the same goal, yet many leave appointments feeling frustrated, misunderstood, or emotionally drained. Families may feel dismissed or unheard, while providers feel constrained by time, systems, and clinical limitations.
This gap is not caused by a lack of care or competence. It is created by emotional load, systemic pressure, and mismatched expectations. Understanding why communication breaks down is the first step toward improving it.
Why Caregivers Often Feel Unseen or Dismissed
Caregivers supporting loved ones with severe mental illness carry far more than symptom updates. They arrive to appointments holding fear, exhaustion, grief, hope, and responsibility. Much of this emotional labor is invisible in clinical settings.
Appointments are often short, problem focused, and driven by immediate clinical needs. When caregivers are interrupted, rushed, or redirected quickly, they may interpret this as dismissal, even when the provider’s intention is efficiency.
Over time, caregivers may stop sharing concerns, minimize their own stress, or leave appointments feeling isolated. This emotional disconnect can impact trust and long term collaboration.
The Emotional Load Providers May Not Realize Families Are Carrying
Many caregivers manage crises between appointments, track behavioral changes, coordinate services, and make high stakes decisions with little guidance. By the time they reach a provider, they may already be overwhelmed.
What providers see as incomplete information or heightened emotion is often the result of cognitive overload. When someone is carrying too much internally, it becomes harder to organize thoughts clearly in the moment.
Without tools or structure, caregivers are expected to recall complex patterns under stress. This can make communication feel scattered or reactive, even when the caregiver is deeply attentive and informed.
How Tools Can Improve Communication
One of the most effective ways to reduce communication breakdown is external structure. When caregivers arrive with organized notes, tracked patterns, and written questions, appointments become more focused and less emotionally charged.
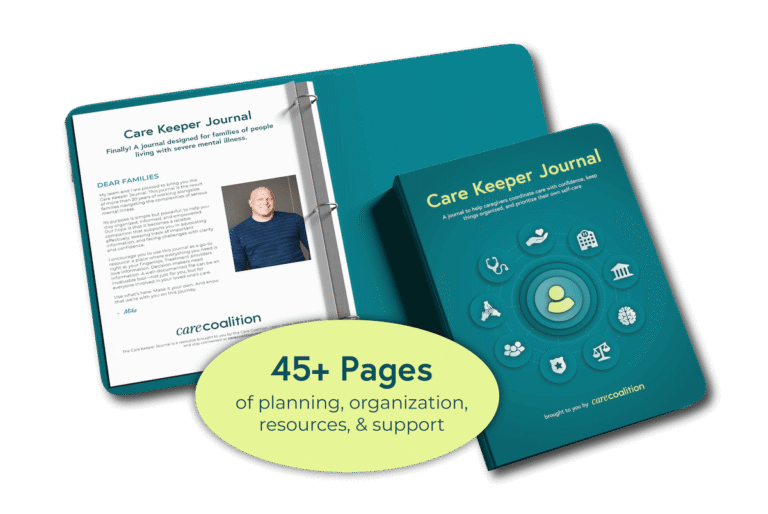
Tools like the CareKeeper Journal were created to support this process. Families consistently share that having a dedicated place to document observations and reflect emotionally reduces anxiety and improves clarity.
For providers, this means more objective data and clearer conversations. For caregivers, it means feeling prepared and heard.
Scripts For More Meaningful Conversations
Sometimes small language shifts make a meaningful difference.
For caregivers:
“I wrote down a few patterns I noticed since our last visit. Can we review the most important ones together?”
For providers:
“I want to make sure I understand what has felt hardest between visits before we talk about next steps.”
These statements set a collaborative tone and acknowledge emotional context without derailing clinical focus.
Five Questions Caregivers Can Bring to Every Appointment
You can save or bookmark these questions to support clearer conversations.
- What changes or patterns matter most for you to know about right now?
- What should we be monitoring more closely between visits?
- How will we know if this approach is helping or needs adjustment?
- What signs would indicate we should reach out before the next appointment?
- What support resources would you recommend at this stage?
These questions create shared understanding and reduce uncertainty for both sides.
Bridging the Gap Moving Forward
Caregivers and providers are not on opposite sides. They are navigating the same complex systems from different positions.
When communication improves, trust strengthens, decisions become clearer, and care becomes more effective. Tools, structure, and mutual empathy are not optional. They are essential.
Care Coalition exists to support this bridge by centering caregiver experience while respecting clinical realities. When families feel supported and providers feel understood, everyone benefits.
Care Coalition strengthens the systems of support around people living with serious mental illness (SMI). Through The Guardian Model™, we equip providers and families with the tools, training, and guidance they need to navigate care more effectively and collaboratively across complex systems.
Copyright Guardian Ac Litem Services, Inc. 2025
Website created by Parker Marketing & Management




